Blog
Diabetic Foot Care: Importance, Tips, and Warning Signs
- posted: Apr. 08, 2024
When you’re dealing with diabetes, you may understand that one of the most important things you can do is care for your feet. For individuals living with diabetes, proper foot Read More
Symptoms of an Ingrown Toenail
- posted: Apr. 01, 2024
Ingrown toenails are painful and ugly. They can make it difficult to put on shoes, to stand, and to walk without pain. An ingrown toenail can decrease your mobility. Your Read More
Treating Plantar Fasciitis
- posted: Mar. 15, 2024
If you are experiencing stabbing, aching heel pain on the side of your foot, or running across your heel, you could have a very common condition known as plantar fasciitis. Read More
Managing Your Heel Pain
- posted: Mar. 01, 2024
Your heels are nature’s shock absorbers, providing a cushion for standing, walking, and running. If you’ve ever experienced heel pain, you already know how it can impact your life. The Read More
The Role of Podiatry in Managing Foot and Ankle Fractures
- posted: Feb. 12, 2024
Foot and ankle fractures are a common problem, especially as you get older. Bones become more brittle, and you are less flexible than you once were. Foot and ankle fractures Read More
Tips for Preventing Heel Pain: Daily Habits for Healthy Feet
- posted: Feb. 05, 2024
At Foot & Ankle Specialists of Connecticut, Dr. Joseph Treadwell and Dr. Christian Davis are the expert podiatrists to turn to when you are experiencing heel pain in Danbury and Read More
Bunions: What They Are and How a Podiatrist Can Help
- posted: Feb. 03, 2024
Foot & Ankle Specialists of Connecticut, staffed by Dr. Joseph Treadwell and Dr. Christian Davis, can provide many podiatric treatments that minimize unnecessary pain and suffering. For example, bunions can Read More
What You Need To Know About Ingrown Toenails
- posted: Feb. 01, 2024
Ingrown toenails can happen to anyone. If you have an ingrown toenail, chances are it’s difficult to put on shoes and want to walk around. Your podiatrist can help with Read More
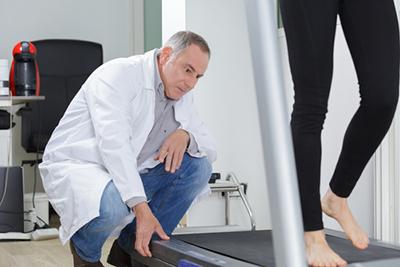
Sports Podiatry: Addressing Foot and Ankle Injuries in Athletes
- posted: Jan. 08, 2024
As an athlete, you know how critical it is to stay at the top of your game and remain in optimal physical shape. Your feet and ankles are the foundation Read More
Orthotics and Their Role in Foot Health: Custom Solutions for Various Conditions
- posted: Jan. 01, 2024
Do you have foot problems? Do your feet hurt all the time? If so, you need to discover the benefits of orthotics. This common treatment, available from your podiatrist, can Read More
Diabetic Foot Care: Preventing Complications and Maintaining Foot Health
- posted: Dec. 07, 2023
Diabetes, a condition affecting how your body uses sugar, impacts various organs, including your feet. High blood sugar can lead to nerve damage (neuropathy) and poor circulation, increasing the risk Read More
Preventing Foot Injuries: Tips for Proper Foot Care and Injury Avoidance
- posted: Dec. 01, 2023
If you experience a foot injury, it can dramatically impact your quality of life. Depending on the injury, foot injuries can lead to loss of mobility, inability to drive, lost Read More
The Benefits of Seeing a Podiatrist
- posted: Nov. 07, 2023
A podiatrist is a specialized medical professional devoted to the diagnosis, treatment, and care of conditions related to the feet, ankles, and lower extremities. Their expertise encompasses many issues, from Read More
The Benefits Of Orthotics
- posted: Nov. 01, 2023
Orthotics are custom-made shoe inserts or insoles designed to support and correct irregularities in foot function. They aim to alleviate various foot and ankle conditions, providing relief and improved mobility. Read More
What To Expect During Plantar Fasciitis Treatment
- posted: Oct. 06, 2023
What to Expect During Plantar Fasciitis Treatment Plantar fasciitis causes persistent, severe pain on your heel and the side of your foot. It’s also one of the most common conditions treated Read More
Our Locations
Danbury
6 Germantown Road, Germantown,
Danbury, CT 06810